Unraveling Multiple Sclerosis: A Comprehensive Guide To MS
Table of Contents
- Understanding Multiple Sclerosis: The Basics of MS
- The Immune System's Misdirection: What Causes MS?
- Recognizing the Signs: Early Symptoms and Progression of MS
- Navigating the Types of Multiple Sclerosis
- Diagnosis and Management of Multiple Sclerosis
- Living with Multiple Sclerosis: Lifestyle and Support
- Advancements in Multiple Sclerosis Treatment and Research
- Global Impact and Awareness of Multiple Sclerosis
Understanding Multiple Sclerosis: The Basics of MS
What is Multiple Sclerosis?
Multiple Sclerosis, or MS, is a chronic neurological disorder that primarily affects the central nervous system (CNS), which includes the brain, optic nerves, and spinal cord. At its core, MS is an autoimmune disorder. This means that the body's immune system, which is normally tasked with protecting us from external threats like viruses and bacteria, mistakenly turns inward. Instead of attacking foreign invaders, it launches an assault on healthy tissues within the CNS. The primary target of this misguided immune attack in Multiple Sclerosis is myelin. Myelin is a fatty substance that forms a protective covering, or sheath, around nerve fibers, much like the insulation around an electrical wire. This myelin sheath is crucial for the rapid and efficient transmission of electrical signals, or messages, between the brain and the rest of the body. When the immune system attacks and damages myelin, it leads to inflammation and scarring, known as lesions or plaques. These lesions disrupt the smooth flow of nerve impulses, slowing down or even blocking messages between the brain and various parts of the body. The term "sclerosis" refers to the hardened scar tissue that forms in multiple areas of the brain and spinal cord as a result of this demyelination process.The Impact of MS on the Body
The damage caused by Multiple Sclerosis can manifest in a wide array of symptoms, depending on which areas of the central nervous system are affected. Since the CNS controls virtually all bodily functions, the impact of MS can be profound and highly individualistic. Common symptoms can include muscle weakness, often affecting one side of the body or a single limb, making daily tasks challenging. Vision changes are also very common, ranging from blurred vision, double vision, or even temporary loss of vision in one eye, particularly due to optic nerve inflammation. Numbness and tingling sensations, often described as pins and needles, can occur in various parts of the body, reflecting nerve damage. Beyond these more common symptoms, MS can also lead to issues with balance and coordination, fatigue that is often debilitating and disproportionate to activity levels, bladder and bowel problems, pain, and cognitive difficulties such as problems with memory, attention, and processing speed. In some cases, MS lesions in certain areas of the brain might trigger seizures, although this is considered unusual given how common lesions are in MS, suggesting other contributing factors are likely at play. The severity of Multiple Sclerosis can range from mild, with infrequent and less impactful symptoms, to severe, leading to significant disability.The Immune System's Misdirection: What Causes MS?
While we understand *what* happens in Multiple Sclerosis—the immune system attacking myelin—the exact cause of this autoimmune malfunction remains elusive. It's widely believed that MS results from a complex interplay of genetic predisposition and environmental factors. It's not directly inherited in a simple Mendelian fashion, but having a close relative with MS does increase one's risk, suggesting a genetic component that makes an individual susceptible. Environmental factors are thought to act as triggers in genetically susceptible individuals. Research has pointed to several potential culprits. For instance, low levels of vitamin D, often linked to reduced sunlight exposure, have been associated with a higher risk of developing MS. Studies suggest that vitamin D has a positive effect on the immune system, and its deficiency might contribute to immune dysregulation. Viral infections, particularly the Epstein-Barr virus (EBV), are also under investigation as potential triggers, though a direct causal link has not been definitively established. Furthermore, lifestyle choices can play a significant role in the disease's progression. For example, people who have Multiple Sclerosis and who smoke tend to have more relapses, worse progressive disease, and worse cognitive symptoms compared to non-smokers. This highlights how external factors can influence both the onset and the trajectory of MS. Gender also plays a role, with women being up to three times as likely as men to develop MS, suggesting hormonal influences. The first symptoms of MS typically emerge between the ages of 20 and 40, a critical period for many individuals establishing their careers and families.Recognizing the Signs: Early Symptoms and Progression of MS
Common Initial Symptoms
The onset of Multiple Sclerosis is often subtle and can be easily mistaken for other conditions. People tend to have their first symptoms between the ages of 20 and 40, making it a disease that often impacts young adults during their most productive years. Early symptoms are diverse and can vary greatly in their intensity and duration. As mentioned, common initial presentations include changes in vision, such as optic neuritis (inflammation of the optic nerve leading to blurred vision or pain with eye movement), double vision, or even temporary vision loss. Sensory disturbances like numbness, tingling, or a feeling of "pins and needles" in the limbs or trunk are also very frequent early indicators. Muscle weakness, often affecting one side of the body or a specific limb, can make simple tasks like walking or lifting objects challenging. Fatigue, a profound and often debilitating tiredness that isn't relieved by rest, is another hallmark symptom that can appear early on. Balance problems, dizziness, and coordination difficulties might also be among the first signs, leading to unsteadiness and an increased risk of falls. Because these symptoms can be intermittent and sometimes resolve on their own, they might not immediately raise alarm bells, delaying diagnosis.Relapses and Remissions in MS
A defining characteristic of Multiple Sclerosis, particularly the most common form, is its pattern of relapses and remissions. Early on, the symptoms tend to get better, sometimes disappearing entirely, only to come back later. A relapse, also known as an exacerbation or attack, is a period when new symptoms appear or existing symptoms worsen significantly. These relapses can last for days, weeks, or even months. They are caused by new areas of inflammation and demyelination in the central nervous system. Following a relapse, individuals typically experience a period of remission, during which symptoms improve or disappear. This improvement can be complete or partial, meaning some residual symptoms might persist. The duration of remissions can vary widely, from months to years. While periods of remission offer relief, each relapse can potentially lead to new or increased neurological deficits, contributing to a gradual accumulation of disability over time. Understanding this fluctuating pattern is crucial for both diagnosis and managing expectations for individuals living with Multiple Sclerosis.Navigating the Types of Multiple Sclerosis
Multiple Sclerosis is not a monolithic disease; it presents in several different forms, each with its own progression pattern. Understanding these types is essential for prognosis and treatment planning. 1. **Relapsing-Remitting MS (RRMS):** This is the most common form of MS, affecting about 85% of people diagnosed with the condition. RRMS is characterized by clearly defined attacks (relapses) of new or increasing neurological symptoms, followed by periods of partial or complete recovery (remissions). During remissions, symptoms may disappear or diminish, and the disease does not appear to progress. However, over time, some residual symptoms may accumulate after each relapse. 2. **Secondary-Progressive MS (SPMS):** Many people who initially have RRMS will eventually transition to SPMS. In SPMS, the disease course changes from a pattern of relapses and remissions to a steady, continuous worsening of neurological function over time, with or without occasional relapses, minor remissions, or plateaus. The rate of progression can vary significantly among individuals. 3. **Primary-Progressive MS (PPMS):** This form of MS affects about 10-15% of people. PPMS is characterized by a gradual, continuous worsening of neurological function from the onset of symptoms, without distinct relapses or remissions. There may be temporary plateaus or minor improvements, but the disease steadily progresses over time. 4. **Progressive-Relapsing MS (PRMS):** This is the least common form, affecting only about 5% of people. PRMS is characterized by a steady neurological decline from onset, but with superimposed acute attacks (relapses). There are periods of continuous progression between relapses. This type is sometimes grouped under PPMS due to its continuous progression. The classification of Multiple Sclerosis helps healthcare professionals tailor treatment strategies, as different types respond differently to various medications and therapies.Diagnosis and Management of Multiple Sclerosis
Diagnosing Multiple Sclerosis can be challenging due to its varied symptoms, which can mimic other neurological conditions. There isn't a single definitive test for MS. Instead, diagnosis relies on a combination of clinical evaluation, neurological examination, and various diagnostic tests. Mayo Clinic's MS care teams, for example, evaluate thousands of people with MS each year, leveraging their concentration on MS and vast experience to make accurate diagnoses. The diagnostic journey typically involves: * **Neurological Examination:** Assessing vision, strength, coordination, balance, reflexes, and sensation. * **Medical History:** Detailed review of symptoms, their onset, and progression. * **Magnetic Resonance Imaging (MRI):** This is a crucial tool, as it can detect lesions (areas of damage) in the brain and spinal cord, which are characteristic of MS. * **Lumbar Puncture (Spinal Tap):** Analysis of cerebrospinal fluid (CSF) can reveal abnormalities like elevated immunoglobulin G (IgG) and oligoclonal bands, which are common in MS. * **Evoked Potentials:** These tests measure the electrical activity of the brain in response to sensory stimulation (visual, auditory, or somatosensory), assessing how quickly and accurately nerve signals travel. Once diagnosed, the management of Multiple Sclerosis is multifaceted, focusing on modifying the disease course, managing symptoms, and improving quality of life. Treatment approaches typically include: * **Disease-Modifying Therapies (DMTs):** These medications aim to reduce the frequency and severity of relapses, slow disease progression, and minimize new lesion formation. They work by modulating or suppressing the immune system. For instance, Siponimod (Mayzent) was approved by the FDA in 2019 for the treatment of active secondary progressive Multiple Sclerosis. The choice of DMT depends on the type of MS, disease activity, and individual patient factors. * **Symptom Management:** Medications and therapies are used to alleviate specific symptoms such as fatigue, spasticity, pain, bladder dysfunction, and depression. * **Rehabilitation Therapies:** Physical therapy, occupational therapy, and speech therapy play vital roles in maintaining function, improving mobility, managing fatigue, and adapting to physical limitations. It is crucial for individuals with MS to work closely with their healthcare team to discuss test results, understand treatment options, and, if desired, learn about their prognosis. As you learn more about Multiple Sclerosis, you may become more proactive in managing your condition.Living with Multiple Sclerosis: Lifestyle and Support
Living with Multiple Sclerosis requires ongoing adaptation and a proactive approach to health and well-being. While there is no cure for MS, lifestyle choices can significantly impact symptom management and overall quality of life. One of the most emphasized lifestyle interventions is physical activity. People with MS can benefit from at least 30 minutes of physical activity at least five days a week. Regular exercise, tailored to individual abilities and limitations, can help improve muscle strength, balance, coordination, and reduce fatigue. Activities like walking, swimming, cycling, yoga, and tai chi are often recommended. However, it's essential to check with a healthcare professional before starting any new routine to ensure it's safe and appropriate. Beyond physical activity, a holistic approach to living with Multiple Sclerosis includes: * **Healthy Diet:** While no specific "MS diet" exists, a balanced, nutritious diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health and energy levels. * **Stress Management:** Stress can exacerbate MS symptoms. Techniques such as mindfulness, meditation, deep breathing exercises, and spending time in nature can help manage stress levels. * **Adequate Sleep:** Fatigue is a pervasive symptom of MS. Establishing a regular sleep schedule and addressing sleep disorders can significantly improve energy levels. * **Avoiding Smoking:** As previously noted, smoking is detrimental for individuals with MS, leading to more relapses and worse disease progression. Quitting smoking is one of the most impactful steps an individual with MS can take for their health. * **Cognitive Strategies:** For those experiencing cognitive symptoms, strategies like using memory aids, breaking down tasks, and engaging in brain-training activities can be beneficial. * **Emotional Support:** Living with a chronic, unpredictable illness can be emotionally challenging. Connecting with support groups, therapists, or counselors can provide valuable emotional support and coping strategies. Sharing experiences with others who understand the unique challenges of Multiple Sclerosis can be incredibly empowering.Advancements in Multiple Sclerosis Treatment and Research
The landscape of Multiple Sclerosis treatment has undergone a revolutionary transformation over the past few decades, offering renewed hope for individuals affected by this condition. What was once a disease with limited treatment options now boasts a growing arsenal of disease-modifying therapies (DMTs) that can significantly alter the disease course. The approval of Siponimod (Mayzent) by the FDA in 2019, specifically for active secondary progressive MS, exemplifies the ongoing progress in developing targeted treatments. This medication works by preventing immune cells from entering the central nervous system, thereby reducing inflammation and nerve damage. Beyond Siponimod, a pipeline of innovative therapies is continuously being researched, including new oral medications, infusions, and injectable drugs that target different aspects of the immune response or even aim to promote remyelination (repair of the damaged myelin). Research into Multiple Sclerosis is dynamic and multifaceted, extending beyond just new drugs. Scientists are exploring: * **Biomarkers:** Identifying specific biological indicators that can predict disease progression, treatment response, or even the risk of developing MS. * **Genetics:** Further unraveling the genetic predispositions to MS to understand who is at risk and why. * **Environmental Factors:** Deeper investigation into the role of viruses, diet, gut microbiome, and other environmental triggers. * **Neuroprotection and Remyelination:** Developing strategies to protect nerve cells from damage and to encourage the body to repair damaged myelin, which could potentially reverse some of the neurological deficits. * **Stem Cell Research:** Exploring the potential of stem cell therapies to repair damaged tissue or modulate the immune system. The collaborative efforts of researchers worldwide, coupled with significant investments in scientific inquiry, are continuously pushing the boundaries of our understanding of Multiple Sclerosis. This ongoing research holds the promise of even more effective treatments, and ultimately, a cure for MS.Global Impact and Awareness of Multiple Sclerosis
Multiple Sclerosis is a complex disease that affects countless individuals around the world. In 2020, approximately 2.8 million people were affected by MS globally, with rates varying widely across different regions. This global prevalence underscores the significant public health challenge posed by the condition. While MS is more common in populations of European descent and in countries further from the equator, it impacts people of all ethnicities and geographical locations. The varying rates suggest that a combination of genetic and environmental factors contribute to its geographical distribution. For instance, countries with higher rates of MS tend to be in colder climates, leading to theories about vitamin D deficiency due to less sun exposure. However, the disease's presence in diverse populations highlights its complex etiology. Raising awareness about Multiple Sclerosis is paramount. Increased awareness can lead to: * **Earlier Diagnosis:** Understanding the early symptoms can prompt individuals to seek medical attention sooner, leading to earlier diagnosis and initiation of treatment, which can significantly impact long-term outcomes. * **Better Support Systems:** Awareness fosters a more empathetic and supportive community for individuals living with MS and their families. This includes advocating for better healthcare access, disability rights, and social services. * **Funding for Research:** Greater public awareness often translates into increased funding for research, accelerating the pace of discovery for new treatments and a potential cure. * **Reduced Stigma:** Understanding the nature of MS can help dispel misconceptions and reduce the stigma often associated with chronic neurological conditions. Organizations worldwide are dedicated to educating the public, supporting research, and providing resources for those affected by Multiple Sclerosis. Oliver Tobien, a neurologist specializing in Multiple Sclerosis at Mayo Clinic, often emphasizes the importance of understanding the basics of MS to empower patients and their families. By continuing to learn about MS, its causes, its different types, and its impact, we can collectively contribute to a future where Multiple Sclerosis is better understood, better managed, and ultimately, cured.Conclusion
Multiple Sclerosis is a formidable chronic neurological disorder, characterized by the immune system's attack on the protective myelin sheath of nerve cells in the brain, optic nerve, and spinal cord. We've explored how this autoimmune process disrupts communication between the brain and body, leading to a diverse range of symptoms from muscle weakness and vision changes to numbness and cognitive challenges. With approximately 2.8 million people affected globally in 2020, the impact of Multiple Sclerosis is far-reaching, often manifesting in individuals between the ages of 20 and 40. Understanding the different types of MS—Relapsing-Remitting, Secondary-Progressive, Primary-Progressive, and the rarer Progressive-Relapsing forms—is crucial for tailored management. While the exact cause remains elusive, a complex interplay of genetic predisposition and environmental factors like smoking and vitamin D deficiency are believed to contribute. However, the advancements in diagnosis, particularly with MRI and CSF analysis, coupled with the development of disease-modifying therapies like Siponimod, offer significant hope in managing the disease and improving quality of life. Lifestyle adjustments, including regular physical activity and stress management, also play a vital role in living well with MS. The journey with Multiple Sclerosis is unique for every individual, but ongoing research and increasing global awareness are paving the way for a future with more effective treatments and, hopefully, a cure. If you or a loved one is affected by MS, we encourage you to engage with your healthcare team, explore available resources, and connect with support networks. Your insights and experiences are invaluable. Share your thoughts or questions in the comments below, and consider sharing this article to help spread awareness and understanding of Multiple Sclerosis. Together, we can make a difference in the lives of those living with MS.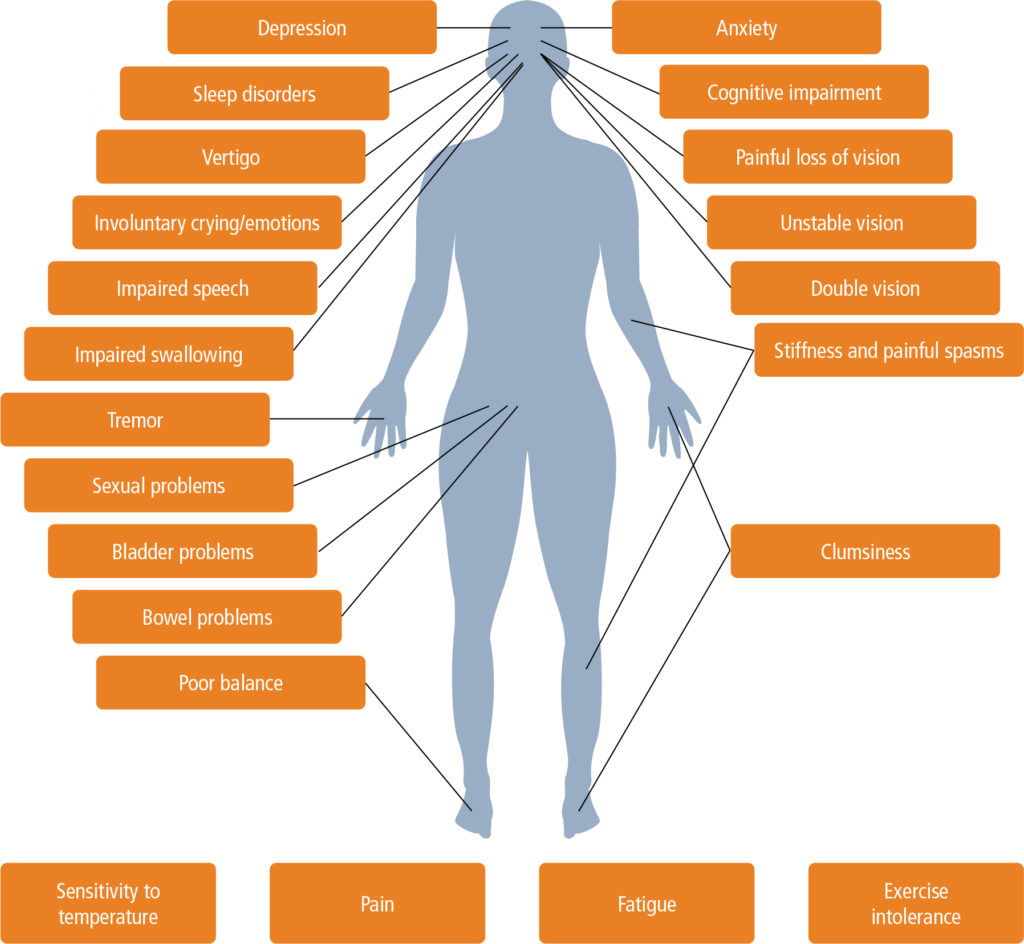
Multiple sclerosis in primary care – diagnosis and early treatment
:max_bytes(150000):strip_icc()/weird-ms-symptoms-and-phenomena-julies-list-2440790_v2-77d3f7200923456480500fd830750433.png)
Ashwagandha Benefits For Multiple Sclerosis / 8 Science Backed Benefits

Multiple Sclerosis